Your pharmacy
at your fingertips!
The World’s First Digital Pharmacy Since 2000
We deliver to your doorstep across Canada.
Why Use our Online Pharmacy?
Delivering the prescriptions you need, the care you deserve
Free Shipping and Savings
Filling your prescriptions with us can save you two dispensing fees for every order (3 months supply) and free shipping delivery to anywhere in Canada.Read More »
Privacy and Security
ADV-Care fills your prescriptions in secure and private packaging, guaranteeing accurate prescription fulfillment. Personal data is private and safeguarded.Read More »
Speed and Convenience
Whether you're at home or away, we'll deliver your medications right to your door so you never have to leave your house or stand in line.Read More »

- We have over twenty years of online experience.
- Provide all branded and generic Canadian drugs.
- Save up to 66.7% of your out-of-pocket expense.
- Directly reach the pharmacist privately during business hours.
- Order your prescription meds online or mobile 24/7.
- Automatic refill reminder to never miss your meds or doctor's appointment.
- We ship anonymously to your home, business or travel destination across Canada
Always Safe and Secure
ADV-Care Pharmacy offers customers bank-level security using IBM technology, with stringent privacy protection for all your personal, medical and financial data. Your privacy and data security are top concerns for ADV-Care! We ensure privacy & security of all patient’s data. Want to learn more? Read our Privacy Policy and Terms of Service.
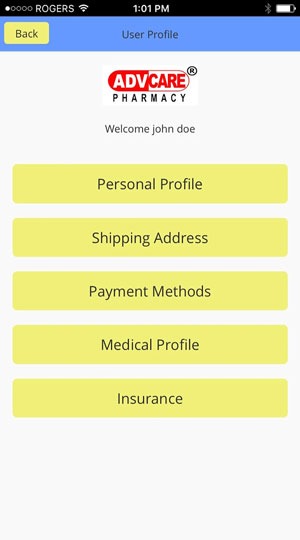
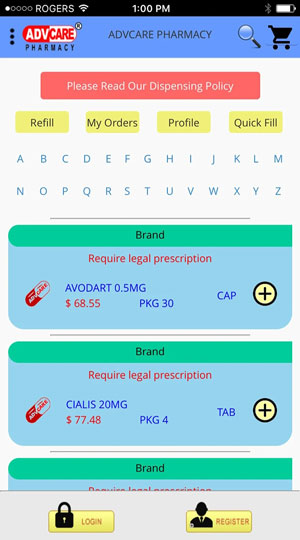
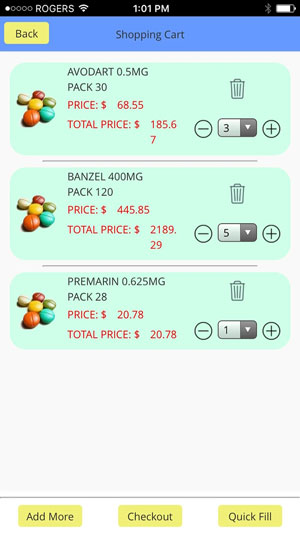
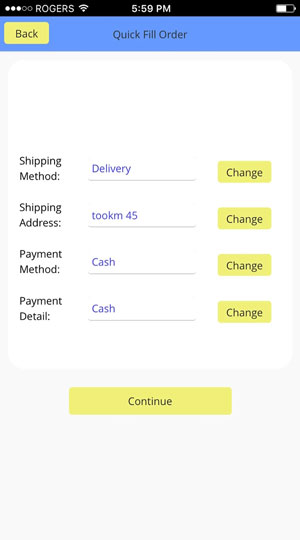
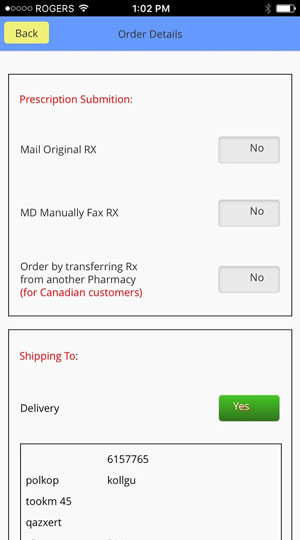
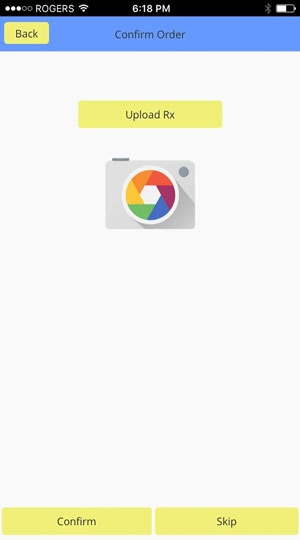
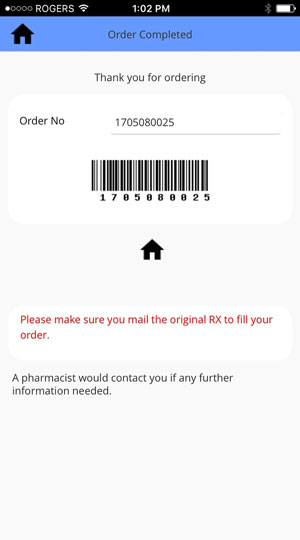
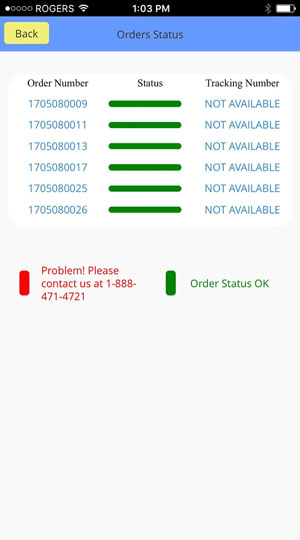
How ADV-Pharmacy Works
Three steps are enough to complete your order
Prescription Drugs
Common Drugs
Products not found.
OTC Drugs
Cold & Flu
Products not found.
Pain / Fever
Products not found.
Hair Care
Products not found.
Skin Care
Products not found.
Allergies / Sleep
Oral Care
Products not found.
Nausea / Vomiting
Products not found.
Quit Smoking
Products not found.
Digestive Care
Products not found.
Foot Care
Products not found.
Disinfection
Products not found.
Minerals
Products not found.
Latest from our Blog

Have you ever had that pain and burning sensation in your chest as you’re just getting ready to sleep...
Medication adherence refers to the extent to which a person’s medication-taking behavior corresponds...
No posts found




